Overview
Therapeutic nanoparticles (NPs) approved for clinical use in cancer patients provide only modest improvements in patient survival, likely due to a number of delivery challenges. The discovery of unique cell surface proteins associated with certain tumors has facilitated new approaches for nanocarrier design and payload delivery; specifically, the capability of targeting and selectively killing tumor cells while sparing healthy tissue. One such protein is the TNF receptor family member fibroblast growth factor-inducible (Fn14). Fn14 is normally expressed at low levels in healthy tissues but is upregulated in over a dozen solid cancer types, including brain cancer (e.g., glioblastoma (GBM)) and triple negative breast cancer (TNBC) - two cancers that are notoriously difficult-to-treat and associated with short patient survival. To overcome the limitations of current nanocarrier technologies and deliver therapeutic agents directly to tumor cells, UMB investigators have designed an innovative therapeutic delivery platform based on Decreased non-specific Adhesivity, Receptor-Targeted (DART) technology. DART formulations are drug-NP complexes that are uniquely engineered with stealth coatings and Fn14-targeting components. This platform technology has unique capabilities to improve therapeutic delivery to Fn14-positive tumors in various locations within the body, increase the maximum tolerated dose of encapsulated drugs, and reduce unwanted side effects and toxicities.
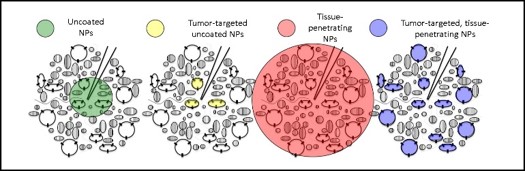
Figure 1. Schematic of DART therapeutic platform technology
UMB investigators have engineered the DART technology to concurrently enable receptor-mediated interactions and minimize non-specific adhesivity to (i) improve nanoparticle blood circulation time and dispersion, (ii) ‘slip through’ and rapidly penetrate tumor tissues in vivo, (iii) promote significantly longer drug retention within the tumor and (iv) overcome MDR transporter-based drug resistance mechanisms (Fig. 1). In one DART formulation, biodegradable poly(lactic-co-glycolic acid)-poly(ethylene glycol) (PLGA-PEG) nanoparticles are conjugated with ITEM4, an antibody specific to Fn14. The DART NP formulation has been characterized and tested in vitro, ex vivo, and in vivo using surface plasmon resonance (SPR), multiple particle tracking (MPT), flow cytometry, confocal microscopy, and near-infrared fluorescence imaging assays, which demonstrate that this technology provides minimal NP nonspecific binding towards blood serum and tumor ECM proteins, and selectively targets Fn14-positive tumor cells. Additionally, DART nanoparticles have been successfully tested in animal models of GBM and TNBC. For example, efficacy studies in an orthotopic MDA-MB-231 TNBC xenograft model demonstrate that paclitaxel (PTX)-loaded, DART NPs (PLGA-PEG-ITEM4-PTX) traffic to Fn14-positive tumors and inhibit tumor growth (Fig. 2). In additional studies using this model, the investigators found that DART NPs outperform Abraxane, an FDA-approved PTX-NP formulation.

Figure 2. (A) Fluorescence image of 231-Luc tumors isolated from mice 24 h after administration of fluorescent PLGA-PEG-IgG or PLGA-PEG-ITEM4 NPs. (B) Analysis of fluorescence intensity from panel A. Values shown are mean +/− SD (n=3). Data analyzed for significance using Student’s t-test. **P < 0.01. (C) Mice with 231-Luc tumors were treated once via IV injection of either saline (black line) or Fn14-targeted DART nanoparticles (red line) and tumor growth monitored over time.
Advantages
Decreased adhesion to non-specific targets
Specific targeting to tumor sites
Longer drug retention and improved biodistribution within tumor microenvironment
Stage of Development
(RB 3/6/24)
Licensing Potential
Available for licensing
Contact Info
Office of Technology Transfer
620 W Lexington St., 4th Floor
Baltimore, MD 21201
Email: [email protected]
Phone: (410) 706-2380