Overview
Lipid A, the hydrophobic anchor of lipopolysaccharide (LPS), can stimulate the innate immune system via Toll-like receptor 4/myeloid differentiation factor 2 (TLR4/MD2), leading to the release of inflammatory cytokines/chemokines and type I interferons. In turn, this response increases the host’s ability to eradicate a pathogen and supports the subsequent development of adaptive immunity. Importantly, the structural variation of lipid A can alter the stimulation ability of LPS via TLR4/MD2. Their role in adaptive immunity has propelled the study of lipid A mimetics as vaccine adjuvants, as a way to increase vaccine efficacy by stimulating immunity against vaccine antigens. UMB researchers have used the normal bacterial LPS biosynthesis pathway in Gram-negative bacteria to synthesize unique lipid A structures based on the presence or absence of specific phosphate, acyl, and carbohydrate groups, to generate novel, rationally-designed Lipid A molecules. This technique, coined Bacterial Enzymatic Combinatorial Chemistry (BECC) can generate structurally distinct lipid A moieities with potential to function as vaccine-adjuvants. BECC method is inexpensive and can yield Lipid A moieties of high purity and yield. These Lipid A species effectively stimulate host’s innate immune system.
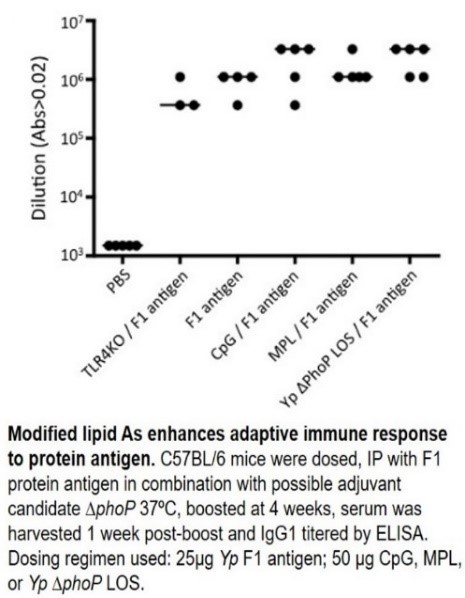
BECC was used to generate a panel of TLR4 agonist molecules that elicit TH1 and TH17 responses with limited endotoxin effects. Unique lipid A-based structures were created in a wide variety of bacterial backgrounds (Yersinia pestis, Francisella novicida,and Salmonella typhimurium). Following the generation of these BECC strains with engineered lipid A modifications, lipid A moieties were isolated, purified, and analyzed to confirm and quantify the individual structures. The resulting lipid A molecules were then tested in an in vitro cell stimulation assay in THP-1 cells. This assay confirmed their effect on TLR4 signaling, as modified lipid A moieties were able to stimulate IL-8, IL-23, and human RANTES, which are hallmarks of TH1 and TH17 pathway activation via TLR4 signaling. In mice, modified lipid A moieties enhanced adaptive immune responses to protein antigens (see figure), confirming their potential as vaccine adjuvants and immunomodulators.
Applications
The global vaccine adjuvants market reached $467 million in 2016 and is expected to grow given the increased focus on immunization programs. One lipid A derivative has been approved for use in the US (monophosphoryl lipid A in Cervarix, 2009). Since then, several TLR4 phospholipid A derivatives have been tested in the clinic and have been shown to enhance TH1 immune responses while being well-tolerated. This platform allows the discovery of novel adjuvants that may be used for research and commercial applications, in prophylactic and therapeutic vaccines, for both human and veterinary health.
Advantages
Easy-to-use BECC platform can screen for novel immunomodulators and adjuvants
Modified lipid A moieties are TLR4-specific agonists
Modified lipid A compounds specifically signal via TH1 and TH17, not TH2, supporting their safety
Stage of Development
Modified lipid A moieties have been tested in an in vitro cell assay and in vivo in mice to assay for their adjuvant potential. The data suggest these moieties effectively stimulate the host’s innate immune system via TLR4 signaling. The activation of TH1 and TH17 effector cells supports their use as safe adjuvants and immunopotentiators, as well as their potential to be administered in intranasal formulations.
(As of 3/16/18)
Licensing Potential
Available for licensing
Available for sponsored research
Contact Info
Office of Technology Transfer
620 W Lexington St., 4th Floor
Baltimore, MD 21201
Email: [email protected]
Phone: (410) 706-2380